Abstract
Background
For relapsed/refractory acute myeloid leukemia (R/R AML), treatments used include high-intensity cytotoxic chemotherapy regimens (HIC); low-intensity chemotherapy (LIC); targeted therapies administered as either a single agent or as part of combination therapy; or venetoclax, often in combination with LIC. As options increase for patients with R/R AML, an understanding of the real-world health care resource use (HRU) and costs associated with different treatment regimens is needed.
Objective
We described HRU and costs associated with HIC alone, LIC alone, and select novel, orally administered therapies (alone or in combination with chemotherapy) to better understand HRU and costs of first salvage therapy for AML.
Methods
This was a retrospective analysis using the IBM MarketScan ® database which contains medical and drug data from ~40 million people annually who are covered by employer-sponsored private health insurance in the United States. The time frame for this claims analysis was 1/1/2017-12/31/2019. HRU and costs were estimated for 5 mutually exclusive treatment groups: HIC alone, LIC alone, gilteritinib, other FLT3 tyrosine kinase inhibitors (TKIs), and venetoclax. Gilteritinib, other FLT3 TKIs, and venetoclax treatments could be single-agent or in combination with chemotherapy. Patients aged ≥18 years at AML diagnosis with continuous health plan enrollment for ≥180 days prior to first AML diagnosis and through start of first salvage therapy were included in the analysis. Evidence of R/R AML was determined by diagnosis code and use of a treatment-based algorithm (Grinblatt DL, et al. Blood. 2020;136[Suppl. 1]:24-25). Descriptive statistics were used to characterize baseline patient demographic and clinical characteristics and HRU and costs through treatment. HRU and costs were reported as per-patient per-month (PPPM).
Results
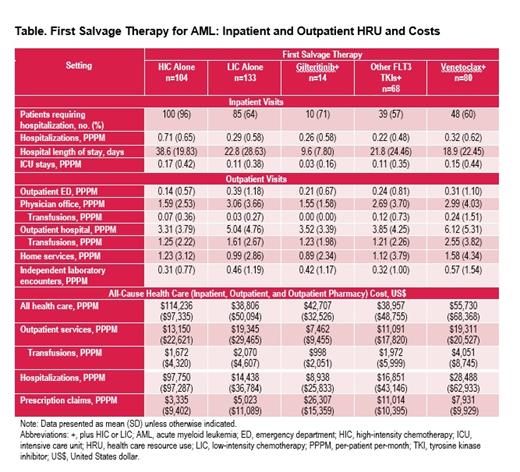
Most baseline characteristics were similar across treatment groups (eg, % male, 45.6%-57.1%; mean Charlson comorbidity scores, 3.07-3.86; and mean all-cause health care costs during 6-months pretreatment, $201,583-$253,437). Mean (SD) patient age overall was 54.1 (14.9) years; the venetoclax group appeared older (61.2 years). The frequency of prior HIC treatment in the overall sample was 38.1%; a majority of patients treated with gilteritinib (64.3%) and other FLT-3 TKIs (55.9%) had prior HIC treatment. Of patients receiving gilteritinib, other FLT3 TKIs, and venetoclax, 6 (42.9%), 33 (48.5%), and 77 (96.3%) respectively, were receiving concomitant chemotherapy. Almost all patients were hospitalized during HIC; the percentage of patients requiring hospitalization was lower and comparable across other treatment groups (Table). Hospital length of stay was highest in the HIC group and lowest in the gilteritinib group. Intensive care unit stays PPPM were highest in the HIC and venetoclax groups and lowest in the gilteritinib group. In the outpatient setting, physician office visits and outpatient hospital visits PPPM were higher in the LIC, other FLT3 TKIs, and venetoclax groups and lower in the HIC and gilteritinib groups (Table). Transfusion-related physician office and outpatient hospital visits PPPM were higher in the venetoclax group than in the other groups. The highest health care costs PPPM were in the HIC group with costs being similar for the other treatment groups (Table). Inpatient costs were highest in the HIC group and lowest in the gilteritinib group; outpatient costs were highest in the LIC and venetoclax groups and lowest in the HIC, gilteritinib, and other FLT3 TKI groups. Transfusion costs in the outpatient setting were the highest in the venetoclax group and the lowest in the gilteritinib group. Prescription claim costs were the highest in the gilteritinib group and lower in the HIC, LIC, and venetoclax groups.
Conclusion
Across select treatments for R/R AML in first salvage, inpatient HRU was generally the highest for the HIC group while outpatient HRU was generally the highest in the LIC and venetoclax groups, with the highest number of outpatient transfusion visits noted in the venetoclax group. Analyses of total all-cause costs showed that costs were the highest in the HIC group and similar in the LIC, gilteritinib, other FLT3 TKIs, and venetoclax groups. Although prescription drug costs were high in the gilteritinib group, these high costs were partially offset by low HRU in both the inpatient and outpatient settings.
Muffly: Adaptive: Honoraria, Other: fees for non-CME/CE services: , Research Funding; Astellas, Jasper, Adaptive, Baxalta: Research Funding; Pfizer, Amgen, Jazz, Medexus, Pfizer: Consultancy. Young: Astellas Pharma, Inc.: Current Employment. Nimke: Astellas Pharma, Inc.: Current Employment. Sullivan: Astellas Pharma, Inc.: Current Employment. Feng: Astellas Pharma, Inc.: Current Employment. Pandya: Astellas Pharma, Inc.: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal